Custom Software Development for Value-Based Care
Technology that supports outcomes, lowers costs, and improves care coordination
Get a free audit
Anonymous Value-Based Care Insights: Key Challenges & IT Solutions
We conducted an anonymous research across healthcare and insurance organizations transitioning to Value-Based Care. Discover the top challenges leaders face — from fragmented data and performance tracking gaps to ROI transparency — and explore proven IT solutions to overcome them.
Learn More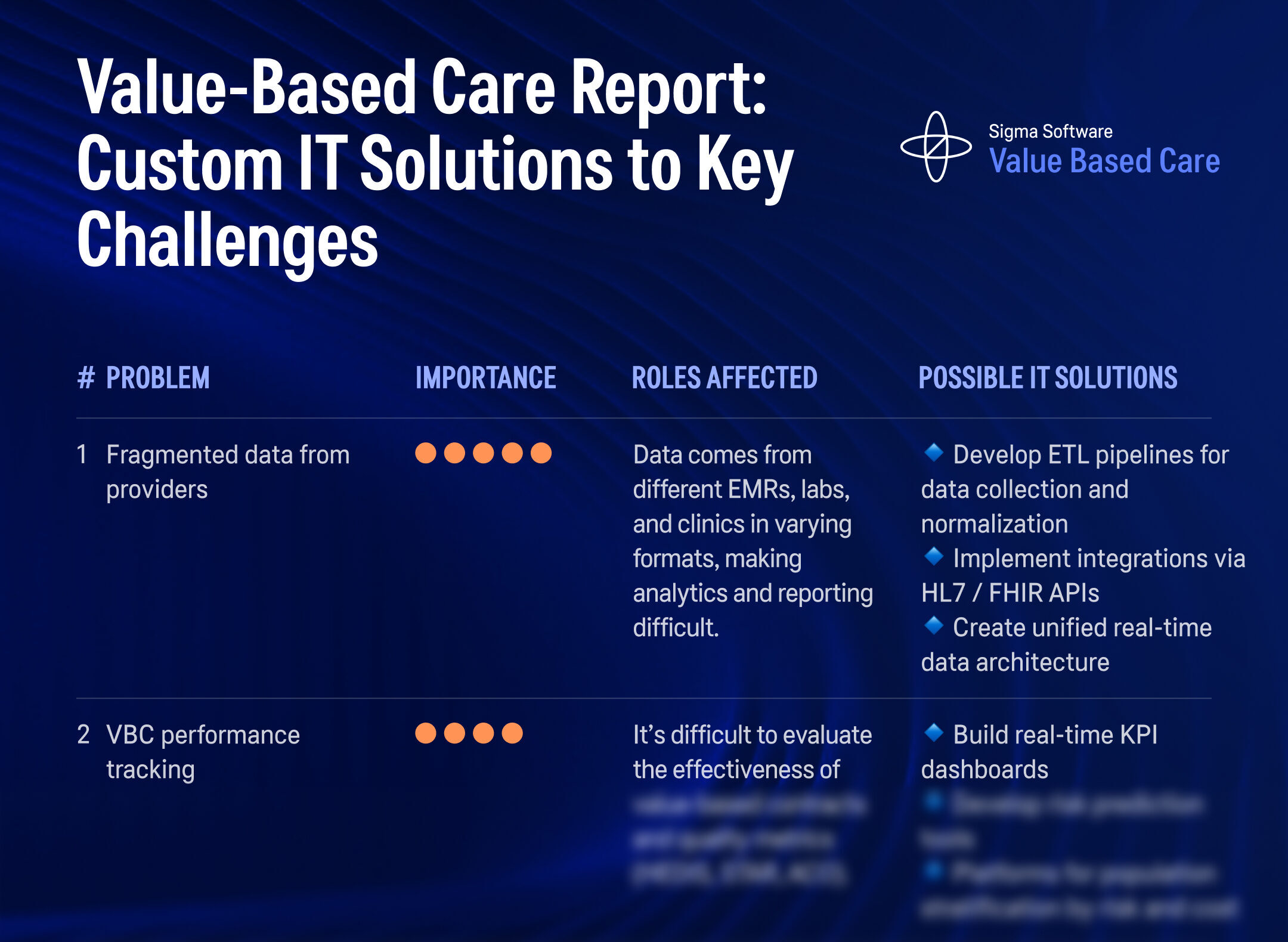
Value based care technologies
Software development for value-based care depends on actionable data, timely interventions, and accurate reporting. To support these goals, organizations need technology that adapts to their structure, contracts, and clinical models. From population health analytics to real-time patient monitoring and predictive risk stratification, custom software makes it possible to improve outcomes, reduce waste, and manage care across teams.
Analytics
Accurate, accessible data is central to managing contracts and improving patient outcomes. Healthcare analytics in value-based care supports providers and payers by identifying patterns in cost, care quality, and patient risk.
Descriptive analytics helps track performance on metrics like HEDIS, STAR ratings, and hospital readmissions. Predictive analytics forecasts which patients are likely to experience adverse events, unplanned utilization, or high-cost episodes. Prescriptive analytics helps align interventions with predicted risk levels, making it easier to act before costs or complications increase.
These systems rely on FHIR integration, HL7 messaging, and strong data normalization practices to deliver insights in real time, supporting more accurate decision-making across the healthcare ecosystem.


Machine Learning and
Computer Vision
Machine learning in healthcare enables more accurate risk scoring, care gap detection, and patient segmentation. These tools help organizations identify who is at risk, which interventions are likely to work, and how to allocate resources more effectively.
In a value-based care model, ML algorithms are used to build risk stratification models, evaluate program performance, and calculate outcome attribution across teams and providers. This is especially important when determining shared savings, adjusting payments, or evaluating the success of care pathways.
ML-based models also help track vendor ROI, by measuring changes in cost or outcome before and after implementation, using real-world patient data.
Real-Time Monitoring
To reduce hospitalizations and improve care after discharge, real-time patient monitoring provides continuous visibility into vital signs, behavior, and medication adherence. These systems connect with remote patient monitoring tools, wearables, and in-home devices, capturing data that helps providers act early.
In value-based healthcare, this helps reduce emergency visits, improve chronic condition management, and close care gaps. Monitoring systems support longitudinal care planning and make it easier to meet contract targets without increasing clinician workload. When integrated with the EHR, this data supports follow-up decisions, compliance tracking, and timely alerts for care teams.


Telehealth
Telehealth in value-based care supports access, continuity, and efficient care delivery. Virtual care tools are used for follow-ups, behavioral health sessions, chronic disease management, and home-based assessments.
These platforms support HIPAA-compliant video consults, structured assessments, and EHR integration. In accountable care organizations and capitated models, telehealth enables timely check-ins, reduces unnecessary visits, and improves documentation for quality reporting. For patients, it makes participation easier. For providers, it supports consistent engagement across a care episode.
Data Infrastructure for Outcome-Based Care Models
A strong data foundation is essential for tracking progress in outcome-based care. Custom software systems support integration with multiple EMRs, lab systems, registries, and claims feeds using HL7, FHIR, and ETL pipelines.
Systems are designed to handle value-based care analytics, automate CMS reporting, and manage compliance across MACRA, MIPS, NCQA, and GDPR. This makes it easier to measure results, attribute outcomes, and track patient journeys across complex delivery networks.
Unified data platforms support real-time processing, making it possible to deliver population health analytics, cost modeling, and intervention impact measurement—all without losing clinical context.
















How We Support Every
Step of the Value-Based Care Ecosystem
Custom outcome-based software development tailored for the real needs of payers, providers, and patients — improving coordination, compliance, and measurable outcomes across the care continuum.
If your organization is working toward more effective care delivery, stronger performance on value-based contracts, or better use of healthcare data, we’re ready to support you with tailored software solutions.
Patient Risk Stratification & Identification
We develop tools for risk stratification in value-based care, combining EHR, claims, and social determinants data to help identify high-risk patients early. Platforms support chronic care planning and align with HEDIS and STAR quality metrics.
Care Coordination Across Providers
Our solutions streamline care coordination platforms that enable team-based care across primary, specialty, and post-acute providers. They support transitions of care, real-time updates, and shared tasks essential for success in value-based care models.
Population Health Management Platforms
We build population health software that integrates clinical, lab, and payer data for cohort segmentation, utilization monitoring, and cost prediction — helping ACOs and provider groups manage performance under VBC contracts.
Outcome Attribution & Shared Savings Models
Custom software supports attribution analytics in value-based care, linking outcomes to specific interventions. This enables accurate shared savings calculation, supports bundled payments, and ensures transparent provider performance tracking.
Compliance & Quality Reporting Automation
We create systems that automate CMS reporting, manage MIPS, NCQA, and other quality benchmarks, and ensure full HIPAA and GDPR compliance. These tools reduce reporting burden while keeping you aligned with evolving value-based healthcare rules.
Member Engagement & Behavior Tracking
We build custom platforms for patient engagement in value-based care, including digital care plans, automated outreach, and behavior tracking. These systems improve follow-up, medication adherence, and reduce preventable utilization.
Payer Systems: Contracts, Claims & Reimbursement
Our tools support payers in value-based care by automating claims, tracking risk adjustment, and managing value-based contracts. They align reimbursement with outcomes and provide shared dashboards for payer-provider collaboration.
Let’s Improve Outcomes, Reduce Waste, and Build Smarter Infrastructure—Together
Solving Real Problems in Value-Based Healthcare with Custom Technology
At Sigma Software, we partner with healthcare organizations to build custom digital platforms that address the most critical challenges in the value-based care ecosystem—from cost attribution and care coordination to member engagement and performance transparency.
Patient Engagement & Adherence Solution for Medicaid Value-Based Programs
Overview:
A Managed Care Organization (MCO) serving Medicaid populations faced high readmission rates and poor adherence to chronic care plans, threatening the sustainability of its risk-based value-based care contracts.
Problems We Solved:
- Low member engagement with care plans
- Lack of digital tools for behavior-driven support
- No visibility into preventable readmissions
- Missed opportunities to improve quality metrics (HEDIS, STAR)
The result:
We built a personalized member engagement platform with built-in risk stratification, multilingual messaging, reminders, and digital check-ins. Integrated with EHR and care management systems, the tool supported outcome-driven care coordination. It increased adherence, reduced avoidable hospital use, and helped the MCO achieve quality benchmarks under value-based reimbursement models.


Vendor ROI & Intervention Impact Platform for Payers
The Challenge:
A national payer working with dozens of vendors across its value-based care ecosystem needed a way to measure which technologies actually delivered improved outcomes and cost savings.
Problems We Solved:
- No standard tools for tracking vendor ROI
- Difficulty linking interventions to health outcomes
- Inability to compare effectiveness across solutions
- Lack of evidence-based decision support for vendor selection
The result:
We created a tailored intervention impact analysis platform that aggregates patient outcomes, financial data, and usage metrics. The system includes A/B testing, before-and-after analytics, and interactive dashboards to measure performance across clinical domains. This enabled payers to select high-performing vendors, justify reimbursement, and strengthen their outcome-based care strategies
Outcome Attribution & Shared Savings Platform for Value-Based Networks
The Challenge:
A regional Accountable Care Organization (ACO) needed to attribute clinical outcomes to providers, track costs across care episodes, and automate shared savings calculations. Manual reporting and unclear attribution models created barriers to collaboration and fair reimbursement.
Problems We Solved:
- No structured data for linking outcomes to care episodes
- Inaccurate provider attribution for shared savings
- Delays in value-based contract performance tracking
- Lack of transparency for participating providers
Our Solution:
We delivered a custom platform that integrates claims, EMR, and quality data to link cost and outcomes at the episode level. It calculates provider-level impact, aligns with CMS value-based care models, and automates shared savings distribution. The system supports accurate attribution, improves transparency, and enables strategic planning based on population health analytics.

Ready to Solve Your Value-Based Care Challenge?
Let’s talk about your unique workflows and design a custom digital health solution that supports outcome-based care, improves population health, and aligns with value-based reimbursement models.
Whether you’re navigating HEDIS metrics, improving care coordination, or optimizing performance-based contracts, we can help.
Request Free contact to discuss solution
or you can book a call right now
Build Your Custom Implementation Plan
Your implementation plan includes integrations, MVP timelines, and long-term support strategies. We build your value-based care solution around real workflows, compliance requirements, and measurable outcome goals.
Launch and Optimize for Outcome-Based Development
Our solutions combine predictive analytics, AI-driven clinical insights, and secure, interoperable data flows. Whether you need compliance tools, shared savings tracking, or a care coordination engine, we align it with your quality metrics, reimbursement goals, and care delivery model.
Ready to Improve Outcomes with Custom Value-Based Solutions?
We design and build custom software for value-based healthcare, built around your data, workflows, and objectives. Whether you need to unify data, support attribution, or track performance across contracts—we’re here to build what works.
Our specialists

Andrii Pastushok
Healthcare Product Management | Value-Based Care Software Solution | Real-Time Integration & Interoperability for Value-Based Care

Julia Buinova
Value-Based Care Software Solution Consultant | Digital Tools to Drive Adoption, Shared Savings & Clinical Impact in VBC

Hanna Tiselko
Value-Based Care Software Solution Consultant | Outcome Tracking, Risk Stratification & ROI Visibility for Payers & ACOs
Checklist for Healthcare Organizations in 2026: Preparing for Value-Based Care
Care Coordination Software: Key to Unlocking Value-Based Care for Providers and Payers
Patient Engagement Solutions for Hospitals: Custom Software to Accelerate Value-Based Care
Preparing for the CMS TEAM Model: Practical steps for payers and hospitals — value based care in us healthcare
Medical Claims Management Software for Value-Based Care: How Insurance Companies Can Simplify the Transition
IoT Healthcare Solution Software Development for Value-Based Care
Understand Your Value-Based Care Workflow
Delivering better outcomes with aligned incentives takes more than off-the-shelf software. That’s why we build custom healthcare solutions for providers, payers, and care organizations working within the value-based care ecosystem.
We keep our collaboration model simple, transparent, and focused on clinical, operational, and financial outcomes from day one.
step 1
You reach out with a challenge
Whether you’re facing fragmented EHR data, delayed quality reporting, gaps in care coordination, or trouble tracking shared savings, you tell us what’s not working.
We take time to understand your care model, your incentives, and your technical landscape.
- Who’s involved: Your operations, clinical, and data teams
- You get: A clear understanding of your goals within a value-based care model


step 2
We Run a Free Interoperability & Compliance Audit
Our team assesses your FHIR and HL7 data exchange readiness, analyze your compliance with CMS and HIPAA, and map out system fragmentation across payers, providers, and population health tools.
- We surface gaps in data integration, identify regulatory risks, and deliver a visual summary of what’s holding your value-based model back.
- You get: A targeted report on interoperability gaps, regulatory compliance, and integration opportunities
step 3
We deliver a strategy and estimate
Based on our audit, we define a tailored architecture and roadmap. Your solution may include FHIR-native APIs, risk adjustment engines, or KPI dashboards for HEDIS and ACO contract monitoring.
- We’ll show you architecture sketches, an MVP roadmap, EHR integration strategies (e.g., Epic, Cerner), and a cost breakdown—with full transparency on what affects ROI.
- You get: A value-focused plan to build exactly what you need—nothing more, nothing less


step 4
We build an MVP or full solution
Our cross-functional team builds in short, testable cycles. Whether it’s a population health analytics dashboard, an outcomes attribution tool, or real-time care coordination software, you stay involved throughout.
- Delivery: Agile sprints with stakeholder demos every 2–3 weeks
- Your role: Validate results, adjust direction, stay in control
step 5
We support and scale with you
Once the system is live, we monitor, support, and optimize it continuously. If you need to scale across care teams, regions, or service lines, we’ll help you expand safely.
- Our support includes SLA-based uptime, performance monitoring, and ongoing compliance updates for MIPS, MACRA, NCQA, and more.
- What you gain: A stable, growing system with measurable results.

Ready to Build the Future of Value-Based Healthcare?
We develop software that connects people, data, and care outcomes — securely and at scale.
Subscribe to the news
be at the top of the information chain – be the first to know the news.
FAQ
Our platforms are designed to support risk stratification, care gap closure, and predictive analytics—tools that directly improve clinical quality metrics like HEDIS, STAR ratings, and ACO benchmarks. Results include reduced readmissions, earlier interventions, and stronger alignment with shared savings contracts.
We implement end-to-end encryption, HIPAA-compliant infrastructure, and strict role-based access controls. Whether cloud-based or on-premise, systems follow best practices for data privacy, audit logging, and regulatory readiness (HIPAA, GDPR, CCPA).
Yes. We specialize in custom integrations with platforms like Epic, Cerner, and Meditech, as well as claims systems and population health tools. We use FHIR APIs, HL7, and X12 standards to connect across silos—without requiring system replacement.
Best-in-class practices, including encrypted backups, network isolation, intrusion detection, and multi-region failover, are applied by default
Absolutely. We build custom dashboards and KPI tools that monitor VBC performance in real-time, track shared savings attribution, and support ACO/MIPS reporting. This includes predictive models, attribution engines, and compliance-ready data exports.
At Sigma Software, we design and build secure, HIPAA-compliant healthcare software for value-based care organizations, health systems, and payer-provider networks across the U.S.
Our tailored solutions support care quality improvement, cost reduction, and real-time clinical decision-making by integrating with your existing systems and enhancing operational efficiency.
Core technology stack includes:
- Predictive analytics for population risk stratification and care forecasting
- Real-time patient data platforms for care management and outcomes tracking
- Machine learning models for readmission risk and chronic disease management
- FHIR and HL7 integration across EHR systems and external partners
- Custom digital tools to support remote care, care gaps closure, and provider performance tracking
We build specialized healthcare platforms for value-based care such as:
- AI-driven clinical risk prediction engines for targeted interventions
- Outcome-based cost analysis dashboards for provider and contract performance
- Cohort analytics platforms for measuring quality and clinical efficiency
- FHIR-based APIs to streamline care episodes and automate reporting
- Computer vision tools for diagnostics and clinical documentation
- Patient engagement systems with digital care plans, reminders, and adherence tracking
Whether you need to integrate fragmented systems, enable shared savings attribution, or build end-to-end tools to track clinical outcomes, our team delivers custom, scalable, and compliant software tailored to the realities of value-based healthcare.
We work directly with health system IT teams, ACO administrators, care management departments, and population health analysts to reduce waste, improve care, and ensure data flows where it’s needed — securely and in real time.